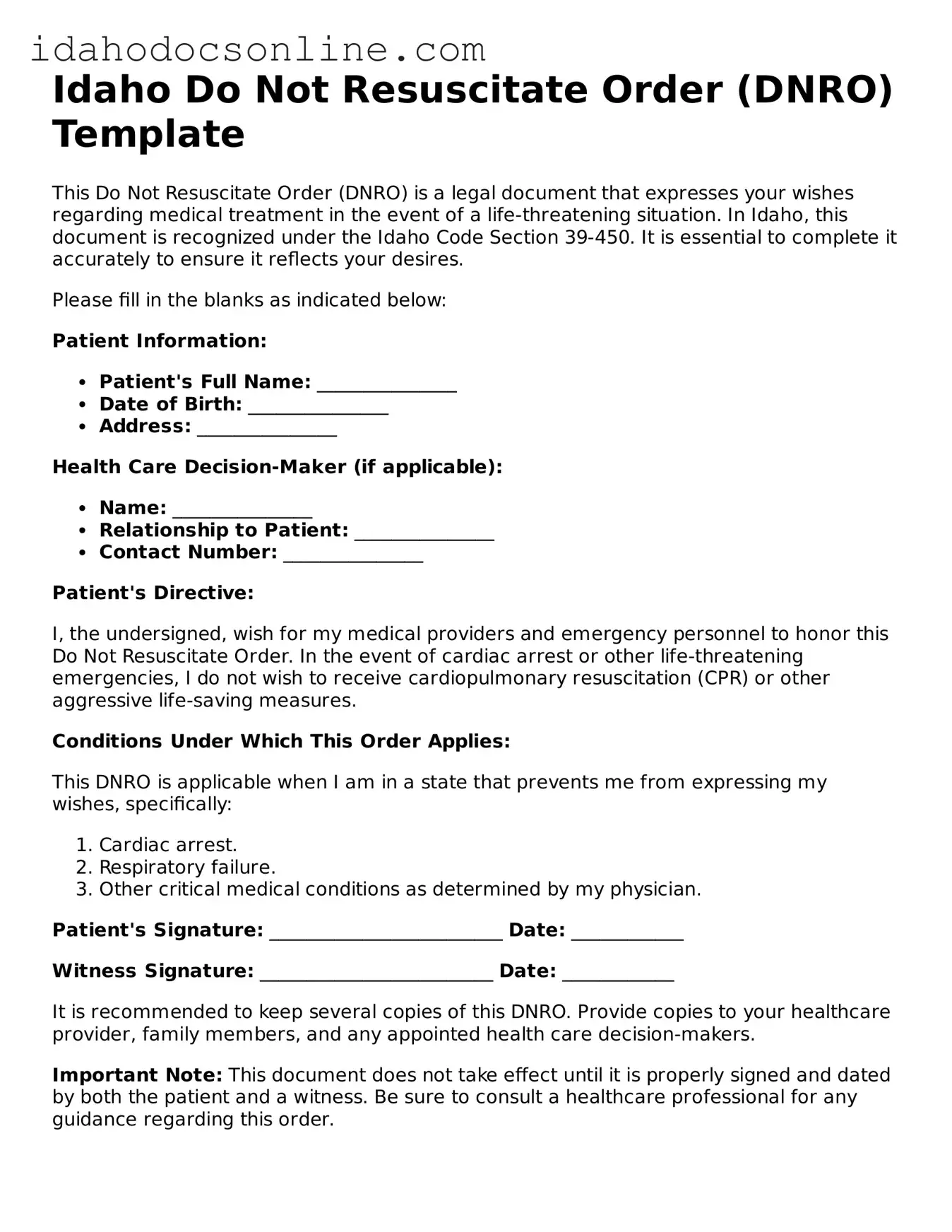
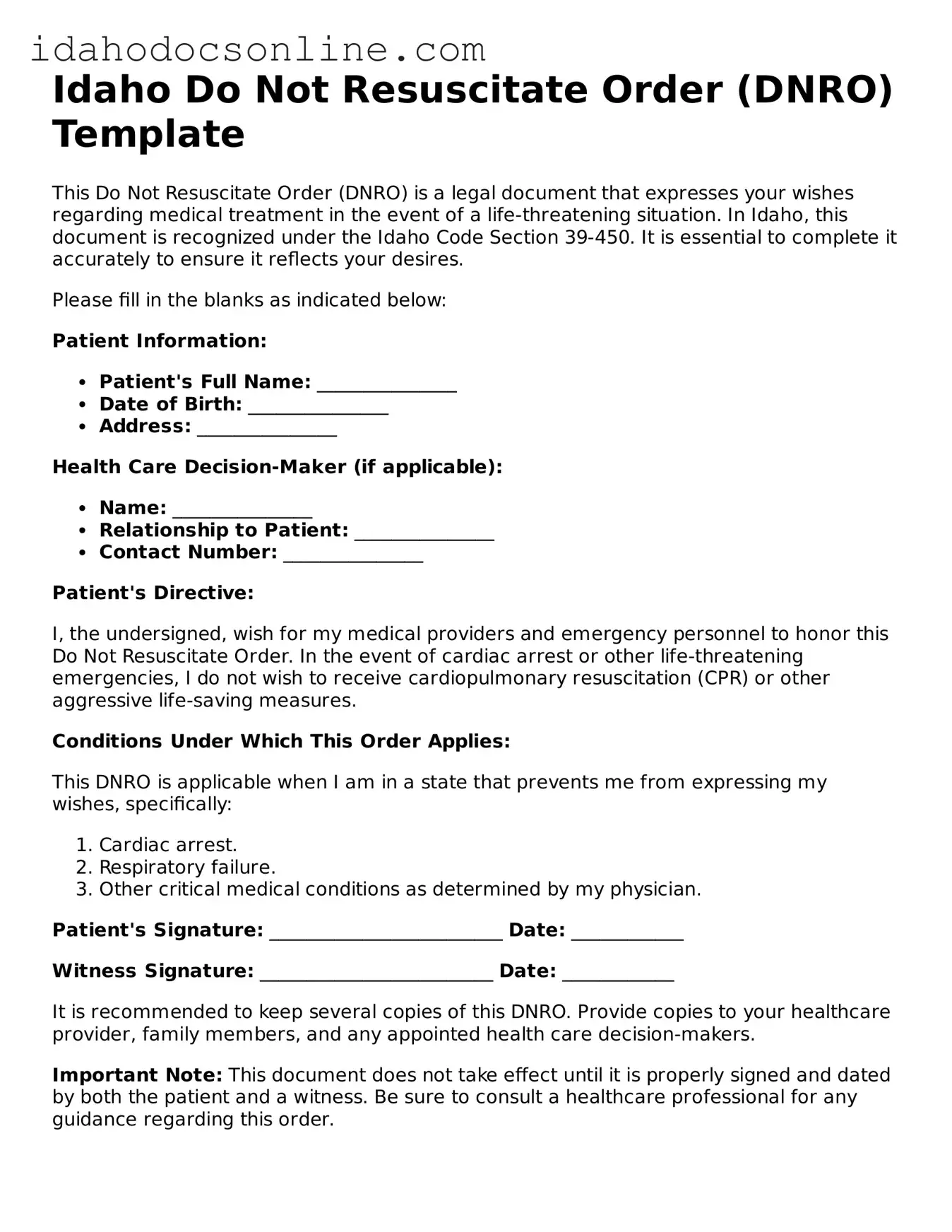
Free Do Not Resuscitate Order Form for Idaho
A Do Not Resuscitate Order (DNR) form in Idaho allows individuals to express their wishes regarding medical treatment in the event of a cardiac arrest or respiratory failure. This legal document ensures that healthcare providers respect a person's desire not to receive life-saving measures. Understanding how to properly fill out this form is crucial for anyone considering their end-of-life care options.
Ready to take the next step? Fill out the form by clicking the button below.
Fill Out Your Document
Free Do Not Resuscitate Order Form for Idaho
Fill Out Your Document
Need speed? Complete the form now
Complete Do Not Resuscitate Order online — edit, save, download with ease.
Fill Out Your Document
or
Free PDF